Overview
More than 1 million Americans survive acute respiratory failure (ARF) each year. These ARF survivors often endure health-related quality of life, physical, psychological, and cognitive impairments in the months following discharge. This shift from short-term mortality to long-term morbidity associated with ARF survivorship stems, in part, from the fact that the robust evidence to guide practice during mechanical ventilation is not matched by similar evidence to guide care after the intensive care unit (ICU) stay. Importantly, 90% of ARF survivors transition from ICUs to general hospital wards during their recoveries, but ward-based threats to ARF survivors’ long-term outcomes and ways to mitigate these threats have not been studied.
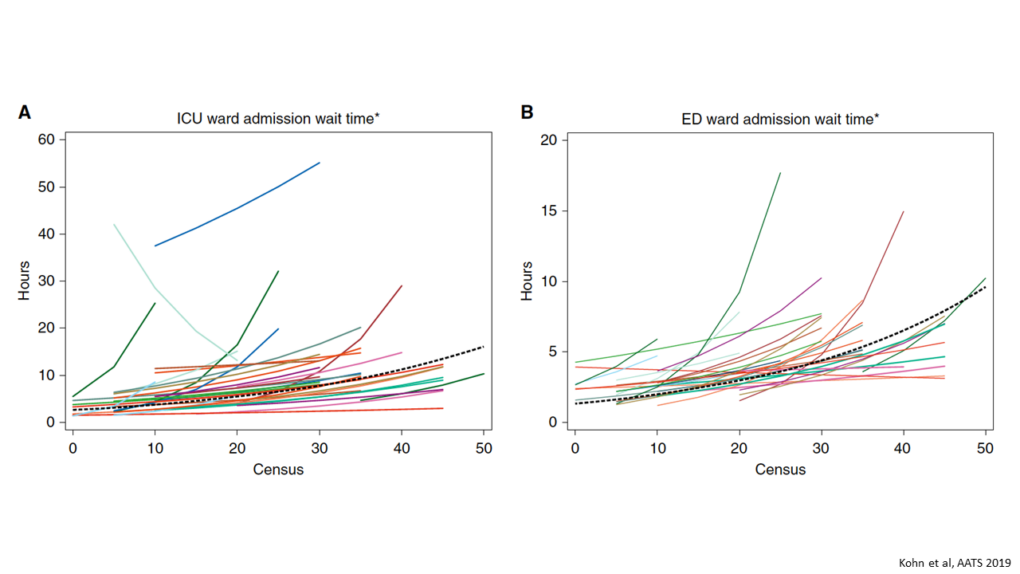
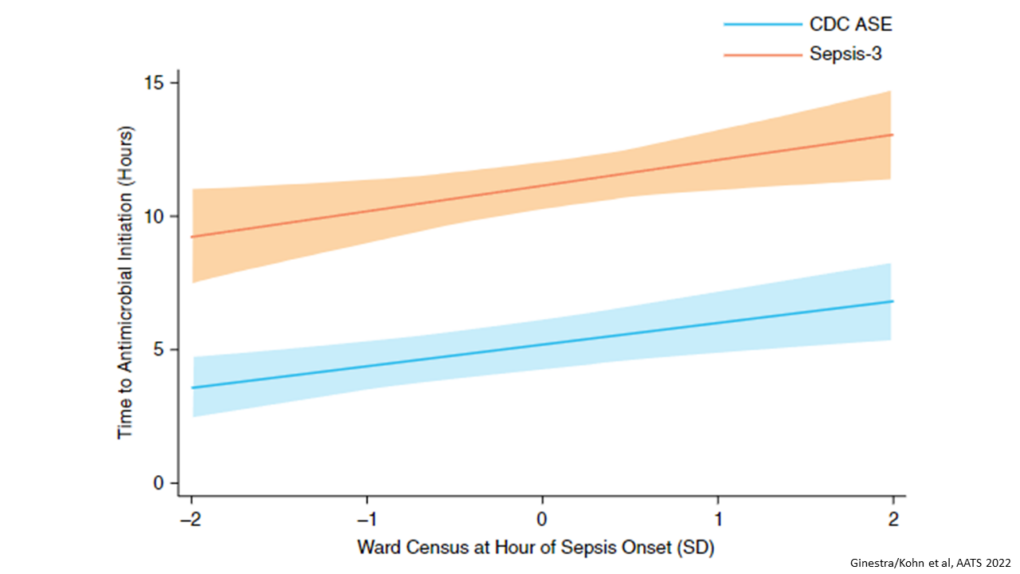
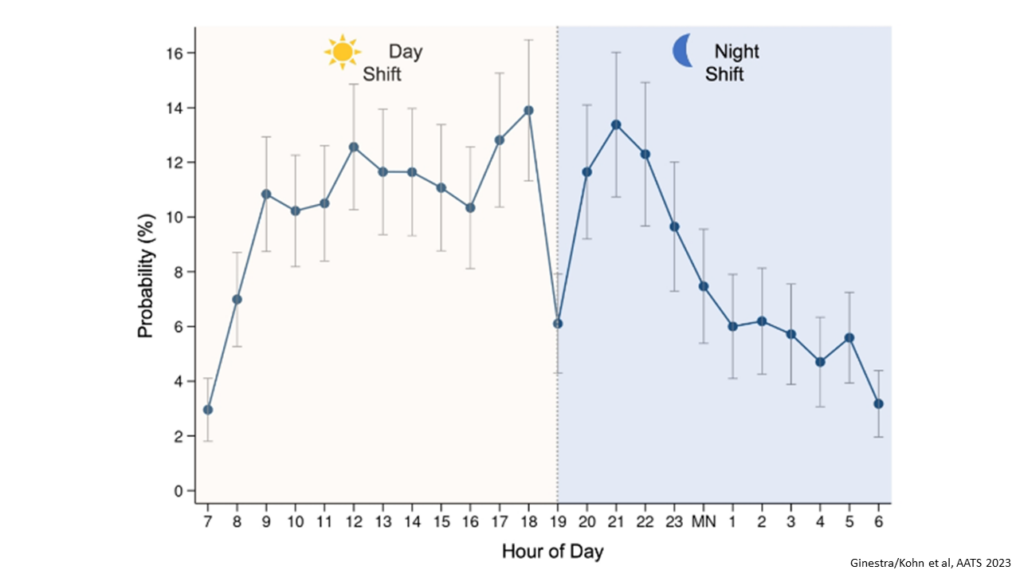
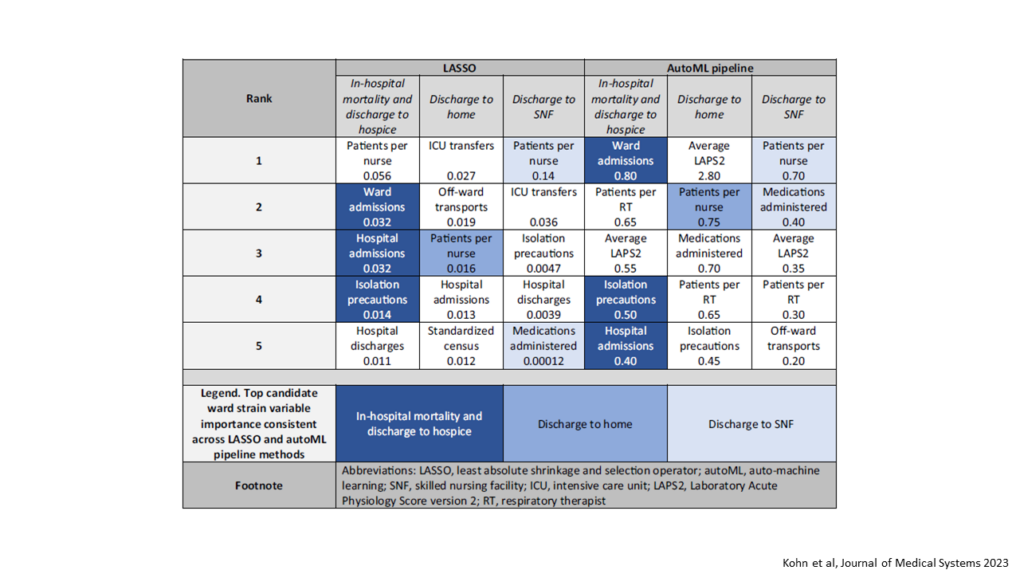
We have defined the construct of “ward capacity strain,” which occurs when demand for ward-based resources exceeds their availability, thus impacting patient care. We identified measures of ward patient volume, staff workload, and patient acuity that contribute to ward capacity strain. We have also defined the construct of “geographic dispersion,” a subset of ward capacity strain, which occurs when patients should be cohorted with clinically similar patients to provide specialized care that improves outcomes and lowers costs, but instead of admitted to alternate locations when these wards exceed capacity.
In addition to the completed studies described below, we have completed enrollment of 100 ARF survivors in a prospective longitudinal cohort study, and are currently completing follow-up. Our objectives are to test associations of ward capacity strain with post-hospitalization clinical outcomes among ARF survivors, and to perform structured interviews with ARF survivors to identify hospital discharge facilitators and barriers to ARF recovery, and to generate hypotheses about discharge practices for this population during times of ward capacity strain.
Results & Impact
We have demonstrated that:
1) Increased ward capacity strain was associated with delays in ICU discharge and 30-day hospital readmissions among critical care survivors;
2) Ward admissions, isolation precautions, and hospital admissions most consistently predict in-hospital mortality; patients per nurse most consistently predict discharge to home; and patients per nurse and medications administered most consistently predict discharge to skilled nursing facilities among ARF survivors;
3) Time to antimicrobial initiation increased with increasing census among ward patients with hospital-acquired sepsis, and at shift changes and overnight; and
4) Pulmonary and general medicine patients who are geographically dispersed have worse clinical outcomes than their cohorted counterparts.
Sponsors
National Institutes of Health, National Heart, Lung, and Blood Institute (NHLBI)