Projects | In Progress
Tracking Recovery in Acute Injury to the Lungs Study (TRAILS)
Research Areas
Principal Investigator
PAIR Center Research Team
Topics
Overview
Post-intensive care syndrome (PICS) can cause serious problems with the body, mind, and memory that may last for months or even years after someone recovers from a critical illness. More than half the people who survive acute respiratory failure (ARF; i.e., people who spend time on a breathing machine in an intensive care unit [ICU]) develop PICS. Because of this, finding ways to prevent or treat PICS could greatly improve recovery, but right now there are no proven treatments.
People with PICS often face the same emotional and psychological struggles as patients with other conditions, such as cancer, lung disease, kidney failure, mental health disorders, and dementia. For these other conditions, there is growing support for dignity-centered care—a type of care that looks at the whole person. This approach focuses on both the illness itself, and on physical ability, emotional and social well-being, life meaning, and spiritual health. Dignity-centered care helps patients feel valued and understood. Research shows this kind of care can reduce anxiety, depression, and distress. What we do not know yet is whether dignity-centered care can prevent or treat PICS in people recovering from ARF and other critical illnesses.
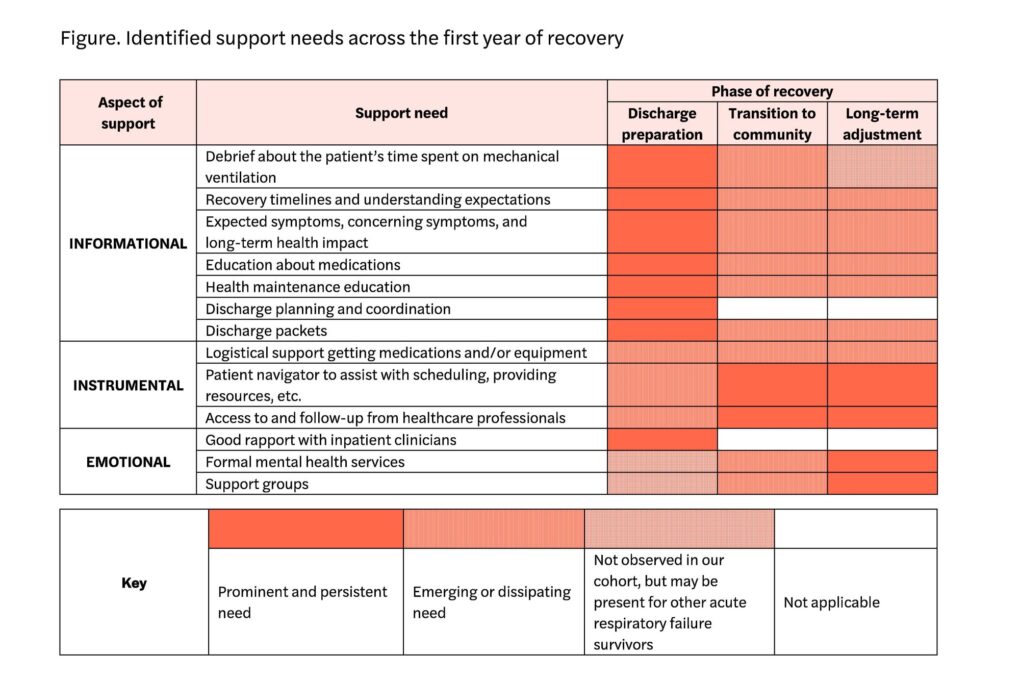
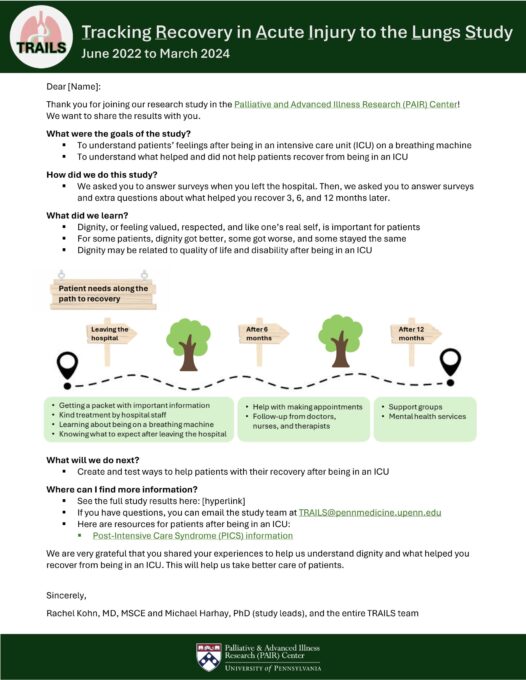
We conducted a study (TRAILS 1.0) to see how problems linked to PICS and feelings of dignity changed over time in people who survived ARF. To measure this, we used standard tools, including the Patient Dignity Inventory (PDI), a 25-question survey that identifies sources of distress related to dignity. In a qualitative study, we also interviewed survivors to better understand their support needs during the first year of recovery.
Our early findings suggest that dignity may play an important role in how well people recover from ARF, and that support needs change during the first year after illness. The current study, TRAILS 2.0, will build on this work by looking more closely at how dignity changes in the first year after hospitalization and what factors influence these changes. This research will provide more data to support a future large, multi-center study of ARF and other ICU survivors. Our goals are to build a model that predicts who will benefit most from dignity-centered care and to test care strategies that improve recovery, moving toward treatments tailored to each survivor’s needs.
Results & Impact
In TRAILS 1.0, we found that patient dignity, measured by the PDI, changed over 12 months among survivors of ARF. These changes were strongly linked with several established domains of PICS, such as quality of life and disability. The differences in dignity scores suggest possible ways to design personalized treatments, but more research is needed to define how dignity changes, understand the reasons for those changes, and test strategies to improve outcomes. Strong links between dignity and physical, cognitive, and psychological measures also show that dignity is a valid way to study ARF recovery, in addition to looking at individual domains of PICS. In our qualitative interviews, we also found that ARF survivors had changing support needs: they needed information at hospital discharge, practical help when moving back into the community, and emotional support as they adjusted over the long term.
Sponsors
National Heart, Lung, and Blood Institute
University Research Foundation