Projects | In Progress
Implementing Nudges to Promote Utilization of Low Tidal Volume Ventilation (INPUT) Study
Research Areas
Principal Investigator
PAIR Center Research Team
Topics
Overview
Background
Each year, about one million Americans experience acute respiratory failure requiring invasive mechanical ventilation. This serious condition can lead to death in up to 30% of patients. A subset of patients have acute respiratory distress syndrome (ARDS), a condition of severe respiratory failure associated with common illnesses like pneumonia and sepsis. One treatment that has been proven to be life-saving for ARDS patients is low tidal volume ventilation (LTVV), which uses smaller artificial breaths on the ventilator to protect the lungs. LTVV may also help patients who are on ventilators but do not have ARDS. However, many patients with ARDS – up to 80% in some hospitals – do not receive LTVV. Research shows that this often happens because ARDS is not recognized, or because clinicians don’t know enough about LTVV or how to use it correctly.
Study Objective
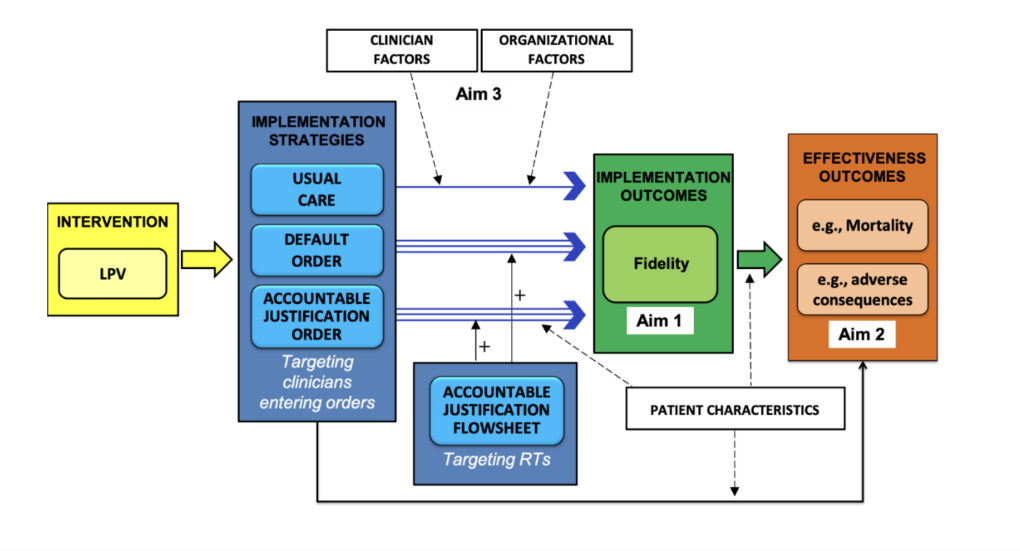
Our goal was to test simple strategies built into the electronic health record (EHR) to “nudge” clinicians toward using low tidal volumes among all mechanically ventilated patients.
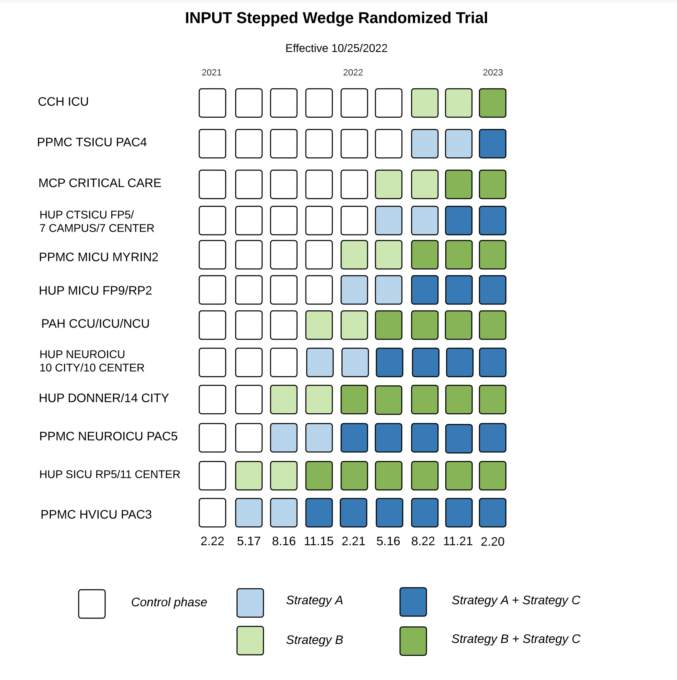
We tested three strategies across 12 ICUs in 5 UPHS hospitals: Strategy A and Strategy B were aimed at doctors, nurse practitioners, and physician assistants. These strategies changed the ventilator order panel in the EHR to make it easier to choose low tidal volumes. Strategy C was aimed at respiratory therapists (RTs), who actually set the ventilator. This strategy required RTs to give a reason if they entered ventilator settings that were not consistent with low volume guidelines
Study Design
We conducted a stepped-wedge, cluster randomized trial. This means that ICUs were randomly assigned to receive one of the physician-focused strategies first. Every three months, two more ICUs started using one of the strategies. Six months after each ICU started, they also received the RT-focused strategy. After all strategies were rolled out, there was a 3-month period where no further roll-outs occurred. This gave us data to compare care before, during, and after the interventions.
To better understand how these strategies worked in real-world settings, we also interviewed doctors and RTs in each ICU during the three months after each strategy was introduced. We asked about their experiences, challenges, and what helped or got in the way of using low tidal volume ventilation.
Partnering Health Systems
University of Pennsylvania Health System (Penn Medicine)
Sponsors
National Heart, Lung, and Blood Institute