Projects | Completed
The Impact of a Global, Race-Free Model for Pulmonary Function Test Interpretation
Research Areas
PAIR Center Research Team
Topics
Overview
Pulmonary function test (PFT) interpretation involves the comparison of observed and predicted measures of pulmonary function. Predicted pulmonary function is based on PFT measurements from healthy individuals, defined as those without a history of tobacco use or respiratory symptoms. Guidelines for PFT interpretation have historically recommend the calculation of predicted pulmonary function using the age, standing height, sex, and race of a patient. Until recently, guidelines for PFT interpretation recommended the use of race-specific reference equations developed by the Global Lung Function Initiative (GLI). In the data used to develop these equations, Black individuals were found to have lower measures of lung function than White individuals when controlling for age, sex, and standing height. The use of these race-specific reference equations to predict normal lung function has led to the widely held idea that a lower measure of lung function on the part of Black individuals is normal. The use of these race-specific equations may thus contribute to lower levels of testing, diagnosis, and treatment of respiratory disease in Black patients.
In this study we sought to estimate the effect the replacement of race-specific reference equations with newly developed race-neutral references equations would have on pulmonary function test interpretation.
Results & Impact
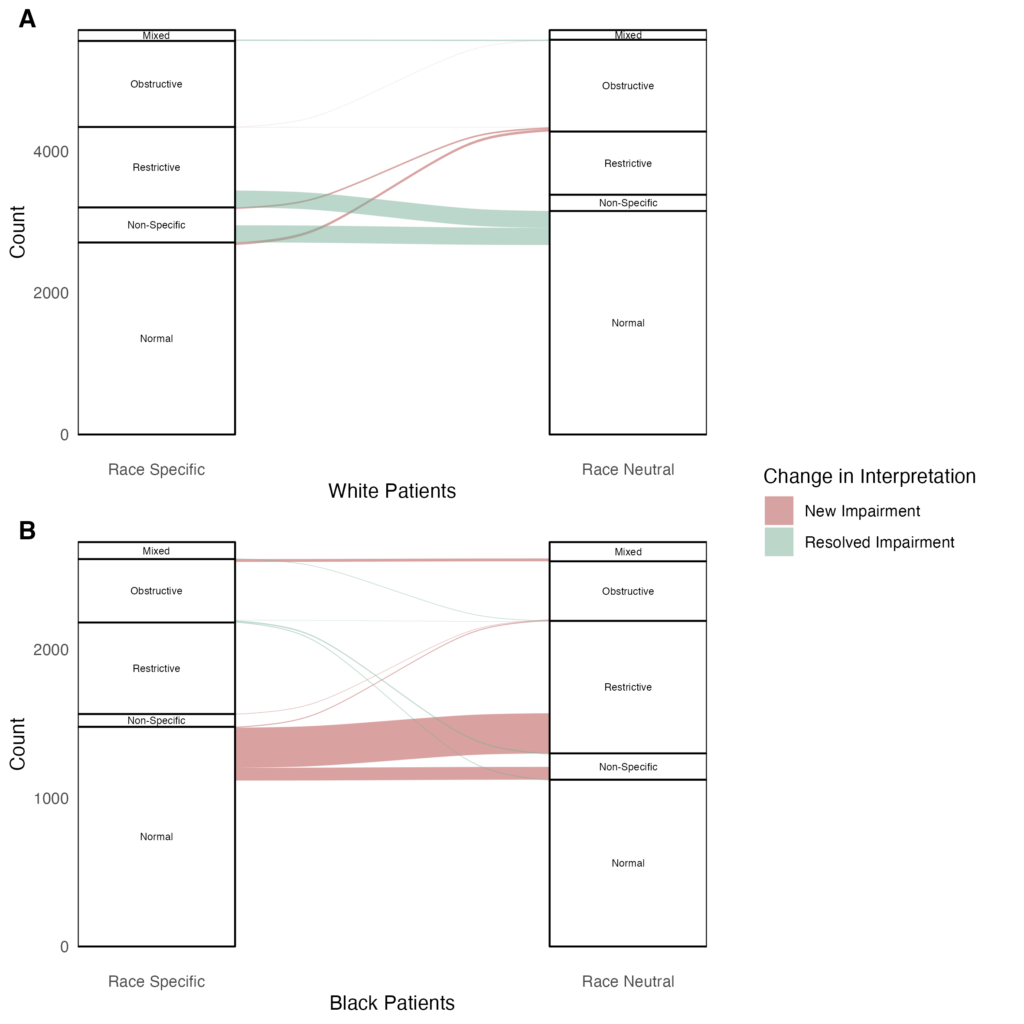
We interpreted PFTs from more than eight thousand patients who had pulmonary function testing performed over a 10-year period at a single academic medical center. We found that replacing the race-specific equations with newly developed race-neutral equations resulted in a significant increase in the number of Black patients found to have restrictive respiratory impairments, from 27 percent of patients to 38 percent of patients. Use of the race-neutral equations led also to an increase in the severity of respiratory impairments in 23 percent of Black patients. In White patients, the race-neutral equations were associated with a decrease in the prevalence of restrictive impairments.
To provide some context for these findings, we noted that if the population of Black individuals who underwent pulmonary function testing in this study were similar to the national population of Black individuals for whom pulmonary function testing is recommended, the application of the race-neutral reference equations at a national level would lead to almost 1 million additional cases of restrictive ventilatory impairments among Black individuals in the United States.
Of note, the American Thoracic Society and European Respiratory Society has recently recommended the replacement of race-specific reference equations with race-neutral equations, so that race no longer plays a direct role in PFT interpretation. The clinical implications of this recommended change are unknown and are an area of active research.
Sponsors
National Heart, Lung, and Blood Institute


